Jurgita Usinskiene (dr. chief radiologist), Kristina Slidevska (radiation oncologist), Audrius Untanas (radiologist); National Cancer Institute, Vilnius, Lithuania
Clinical Challenge: Artificial Intelligence-Powered Prediction of Prostate Cancer Treatment Response After Radiation Therapy
Prostate cancer remains a significant health challenge, with treatment strategies continuously evolving to improve patient outcomes. However, there is no precise tool to predict responses to treatment based on diagnostic imaging radiomic features.
Radiation Therapy for Prostate Cancer
Radiation therapy, a non-interventional treatment, can be utilized in several scenarios:
- As the first treatment for cancer confined to the prostate gland, especially for lower-risk cases. Cure rates for these cancers are comparable to those treated with radical prostatectomy.
- In combination with hormone therapy for higher-risk cancers that are still localized within the prostate or have spread to nearby tissues.
- If surgery is incomplete or if the cancer recurs in the prostate area post-surgery.
The primary types of radiation therapy for prostate cancer are external beam radiation (EBRT) and brachytherapy (internal radiation).
External Beam Radiation Therapy (EBRT) EBRT involves focusing radiation beams on the prostate gland from an external machine. The most common form, Intensity-Modulated Radiation Therapy (IMRT), uses a computer-driven machine that moves around the patient, delivering radiation from multiple angles. IMRT allows adjustment of beam intensity to limit radiation exposure to nearby normal tissues, enabling higher doses to the cancerous area. IMRT is often combined with Image-Guided Radiation Therapy (IGRT), where imaging tests guide precise radiation delivery, potentially reducing side effects.
A variant of IMRT, Volumetric Modulated Arc Therapy (VMAT), delivers more tightly focused treatments in significantly shorter times. At our facility, all prostate cancer patients undergoing radiation therapy receive VMAT.
The Promise of AI in Prostate Cancer Management
Traditional assessment methods for prostate cancer treatment response rely on clinical evaluation, imaging, and biopsies. These can be invasive, time-consuming, and sometimes fail to provide a comprehensive picture of the tumor’s response to therapy. Artificial intelligence (AI) offers a transformative approach, leveraging advanced algorithms and extensive datasets to analyze complex imaging data from multiparametric MRI (mpMRI) scans.
ProCAncer I is an innovative project harnessing AI to predict treatment responses using an international data platform comprising prostate cancer mpMRI, PSA levels, and other clinical variables. This approach has the potential to refine therapeutic strategies early and enhance patient care.
How It Works
The process involves collecting imaging and clinical data into a cloud-based platform. High-quality mpMRI images of prostate cancer patients before and after radiation therapy are input into AI models trained to detect subtle changes in the tumor and surrounding tissues. The AI model, learning from international data that includes patients with and without biochemical relapse post-radiation therapy, analyzes parameters such as tumor size, shape, texture, and molecular characteristics to predict treatment response. The AI model’s output indicates either disease-free status or relapse.
Benefits of Early Intervention
A significant advantage of AI-driven treatment response prediction is the ability to intervene early. If the AI model suggests a poor response to radiation therapy, clinicians can promptly adjust the treatment plan. This may involve switching therapies, increasing radiation doses, or integrating additional treatments like hormone therapy. Early intervention can lead to better outcomes and reduce cancer recurrence risk.
Enhancing Patient Comfort and Resource Allocation
AI predictions can reduce the need for invasive procedures, improving patient comfort and experience. Additionally, healthcare resources can be allocated more efficiently, ensuring appropriate treatments without unnecessary delays or expenses.
The Future of Prostate Cancer Treatment
As AI technology advances, its applications in prostate cancer treatment are expected to grow. This project represents a significant step towards more personalized, precise, and effective cancer care. Integrating AI into clinical practice can lead to treatment decisions guided by data-driven insights, resulting in better patient outcomes and more efficient use of medical resources.
Case Studies
Case No. 1
- Patient Details: Elevated PSA (6.49 ng/mL), Gleason score 4+3=7, DRE – T3b.
- Diagnosis: mpMRI revealed a PI-RADS 5 lesion on the left side (Fig.A)
- Treatment: Radiotherapy combined with hormone therapy in 09-2021.
- Outcome: Follow-up mpMRI in 05/2023 showed no local recurrence. (Fig.B)
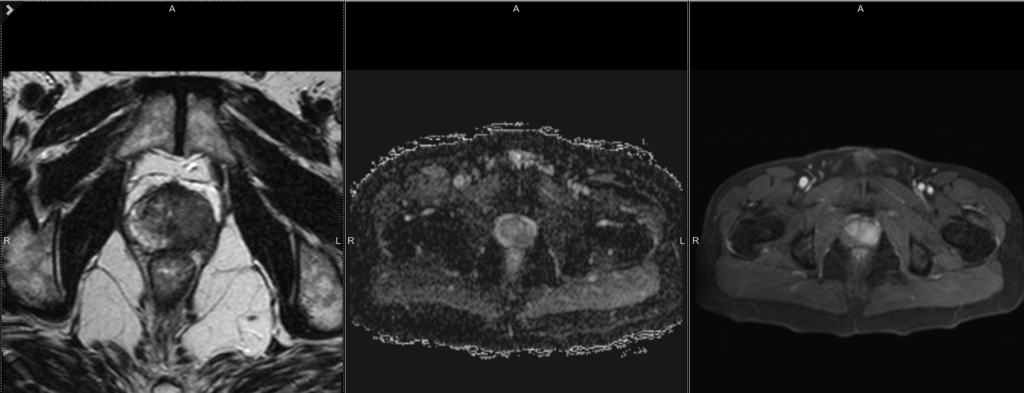
Fig.A
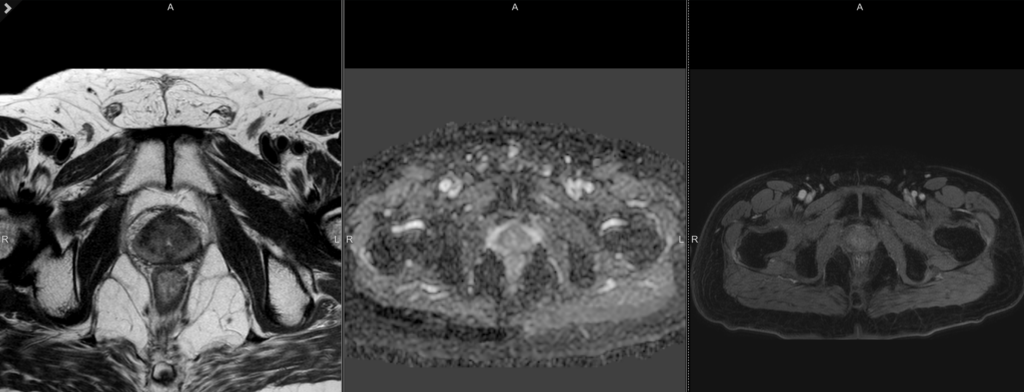
Fig.B
Case No. 2
- Patient Details: Elevated PSA (5.8 ng/mL), Gleason score 3+4=7, DRE – T2.
- Diagnosis: mpMRI revealed a PI-RADS 4 lesion on the left side. (Fig.C)
- Treatment: High-Dose Rate (HDR) brachytherapy in 05/2020.
- Outcome: Follow-up mpMRI in 02/2024 diagnosed disease relapse. (Fig.D)
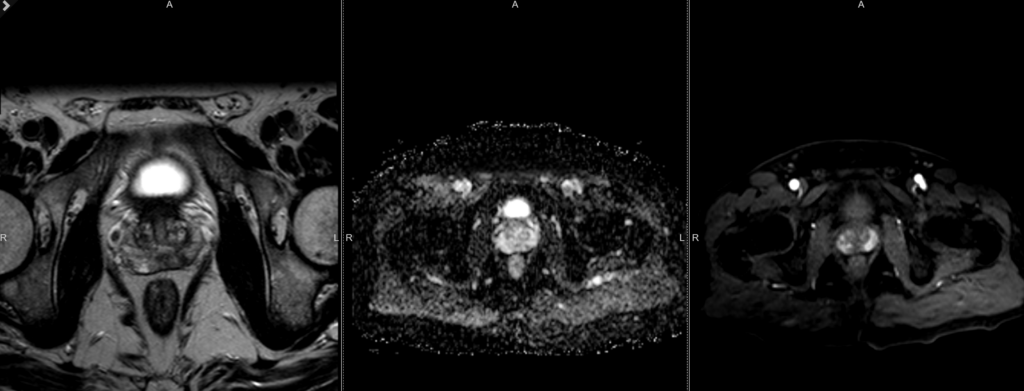
Fig.C
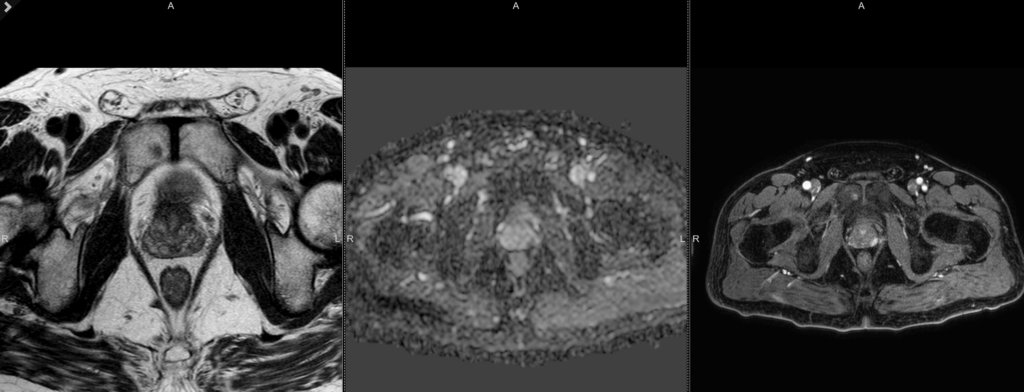
Fig.D
Conclusion
The integration of AI in predicting prostate cancer treatment responses following radiation therapy holds immense promise. By enabling early evaluation of treatment efficacy and allowing timely adjustments in therapeutic strategies, this project aims to enhance patient care, reduce discomfort, and optimize the use of medical resources.



